Scientists have shown that mutations present in circulating tumor DNA isolated from the blood predicts the likelihood a patient will respond to checkpoint inhibitor immunotherapies, indicating that a simple blood test could inform clinicians on whether to administer these treatment regimens.
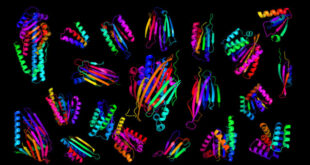
For the first time, researchers have used mutations detected in circulating tumor DNA drawn from patient blood to predict responses to immunotherapy, supporting the usage of this non-invasive diagnostic approach in the clinic. Image credit: National Human Genome Research Institute.
The vast differences between tumors of individual patients cause a broad range of responses to each therapy. Patient tumors often need to be directly biopsied to determine whether a given treatment should be used, a process that can be invasive and sometimes impossible.
Circulating tumor DNA (ctDNA) is DNA that is released into the blood by the tumor.
ctDNA can be isolated from the blood of a patient and sequenced to reveal mutations present in the original tumor, acting as a ‘liquid biopsy.’
Researchers from the University of San Diego School of Medicine were able to predict patient response to checkpoint inhibitor immunotherapy from the appearance of genetic aberrations in patient ctDNA.
“Checkpoint inhibitor immunotherapy is exciting, but it is currently given to patients with all types of cancer, and most of the time it is not known if it will result in a response,” said Razelle Kurzrock, MD, the senior author of the study appearing in the journal Clinical Cancer Research.
“Indeed, more than 80% of patients with cancer fail to respond to checkpoint inhibitor immunotherapy.”
Dr. Kurzrock and colleagues analyzed ctDNA from 69 patients from a wide-range of cancer types that were being treated with checkpoint inhibitors.
Patients that had ctDNA containing many genetic mutations had a longer progression free survival after this therapy.
“Tumors that have the most mutations, and used to be considered the worst tumors, are now considered the best cancers in that they are the most amenable to treatment with immunotherapy,” Dr. Kurzrock said.
Although the relationship between number of mutations in biopsied tumors and immunotherapy response was already established, this study was the first to show this effect could be mirrored in ctDNA from the blood.
“We can take a simple blood sample, which is less painful, less expensive and can be repeated to determine who is at an increased chance of response to immunotherapy,” Dr. Kurzrock said.
“This technology opens up a whole new approach to immunotherapy.”
Dr. Kurzrock is already apart of testing liquid biopsy approaches in the Profile Related Evidence Determining Individualized Cancer Therapy (PREDICT) clinical trial.
In the future, analysis of ctDNA isolated from a trivial blood test could serve as diagnostic tool to inform treatment of cancer patients.
_____
Yulian Khagi et al. 2017. Hypermutated Circulating Tumor DNA: Correlation with Response to Checkpoint Inhibitor–Based Immunotherapy. Clinical Cancer Research 23 (19): 5729-5736; doi: 10.1158/1078-0432.CCR-17-1439
 #Bizwhiznetwork.com Innovation ΛI |Technology News
#Bizwhiznetwork.com Innovation ΛI |Technology News